Initiatives and Projects
Formal medical education begins and ends with teamwork and communication. Medicine allows as a clear focus of our attention...the patient. Surgery is especially dependent on teamwork to ensure a smooth deployment of patient centered, technically proficient, and keen clinical decision making. As the clinical and education background environment in medical training becomes more complex, it is most important to train together and be mindful of the patients and learners at the center of all our efforts.
Senior resident taking a junior resident through a case. University of Missouri Kansas City
Autonomy in the Operating Room
Residents operate in the operating room with various degrees of autonomy. What constitutes autonomy for residents is sometimes vastly different than what an attending construes it as. A mixed methods study is underway in observation of the cholecystectomy undergoing two different techniques and when, how, and why residents are given the reins of the operation. General surveys have been deployed to set the context. Direct case observations of robotic and laparoscopic cases between different dyads of residents and attendings will quantitatively fill in the picture.
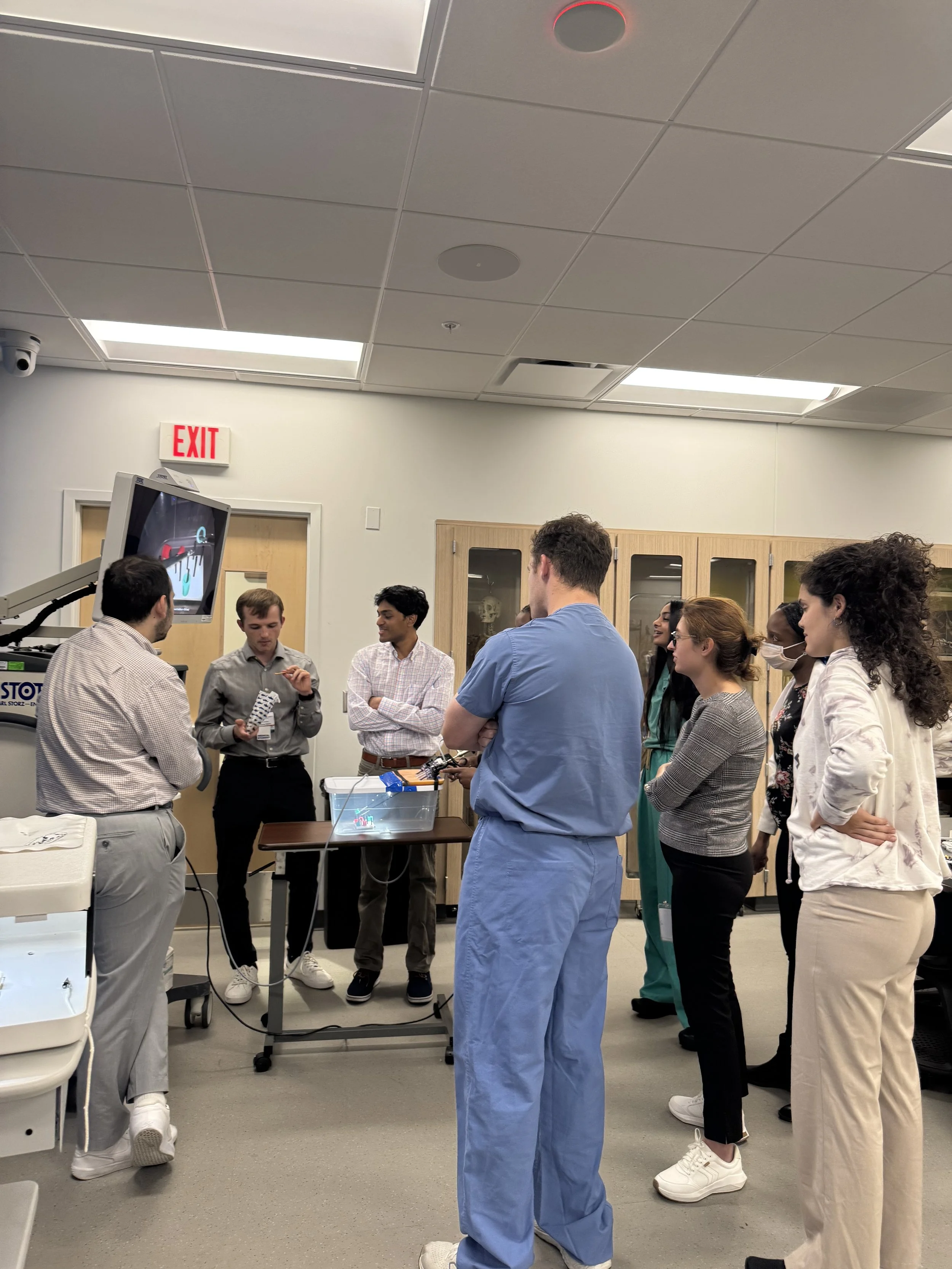
Medical students discuss the educational environment and will set expectations with their teams after this session. University of Missouri Kansas City
Setting Expectations in the Surgical Core Clerkship
Goals and objectives are sometimes cross between students and their resident/attending teams. Setting expectations at the beginning of the core clerkship may help establish a more collegial working relationship that reaps the benefit of a context of caring. A mandatory expectation setting sheet is expected to be reviewed and spark a conversation about student goals for the clerkship and team expectations for the work day/week. Preliminary survey data of students whom had expectations required and those that did not show more confidence in non-technical skills by those that did. Psychological safety was a common thread through the themes of support and role clarity in those that set expectations in the core clerkship.
Screen shot of mistreatment trigger video utilized in the Mistreatment Program for the Surgical Core Clerkship at Stanford
Combating Medical Student Mistreatment
Medical student mistreatment is ubiquitous in various learning environments in medical school. Most commonly tracked and reported to and by the AAMC graduation questionnaire this phenomena can adversely affect students and their ability to learn in the clinical workplace portion of their education. A ubiquitous mismatch of communication and expectations are often at the heart of this learning environment challenge. The student mistreatment program is in-bedded within the core surgery curriculum. The mistreatment program utilizes videos for discussion in week 1 of the clerkship to empower the students for advocacy and reporting.